40 trillion microbes in your gut – this can be more than the combined population of such 5000 earths. What gut microbes are producing says a lot of your health. Microbial population existing symbiotically in different sites of our body constitutes the microbiome, a vital health determinant overlooked. When we are affected by a chronic ailment, we blame so many things, our genes, our environment and our lifestyle. But we do not think of gut biome.
Your gut biome impacts your mind, body and overall health even your brain. Our approach to wellness needs rethinking. Of late, researches on the microbiome have been flourishing. Scientists are gathering more insights regarding the varied metabolic activities of intestinal microbes which could be the checkpoint of many ailments.
A guide on gut microbiome and its role on our well-being
-
How is each man’s “gut” unique?
-
Gut health and wellness: How is it linked?
-
How to let food be thy medicine?
-
How does gut biome support your health?
-
How gut biomes may influence your immune response?
-
How is gut health and your heart is connected?
-
How does gut biome have lots to do with your obesity?
-
Control of blood sugar lowering the risk of Diabetes:
-
How is the gut-brain connected?
-
How can a mother’s microbiome affect brain development in kids?
-
Do you have a healthy gut?
-
Personalized nutrition – How is it the key to a healthy gut?
-
Why take more of Probiotics and prebiotics?
-
How does Lactobacillus have high potential in boosting immune response and restoring gut homeostasis?
-
Why physical exercise?
-
What are the other ways to restore your gut health?
-
What is deep Transcranial Magnetic Stimulation
How is each man’s “gut” unique?
“All disease begins in the gut”, said Hippocrates 2000 years ago. Recent findings are pointing to this fact. Most diseases, if not all have a correlation with our gut. Even though humans share 99% of the DNA, wide diversity exists in gut microbes. Every individual has a unique gut biome that reacts and responds differently towards food.
An apple a day may keep a doctor away from you but not from your friend. The digestion and assimilation process differs in individuals owing to the varied composition of intestinal flora. Gut biome is the cornerstone of our health. Sadly enough, the huge battalion dwelling in our body fighting invaders have received little or no recognition till date. On the contrary, we have been waging war against them unknowingly. How about antibiotics?
Gut health and wellness: How is it linked?
You inherit your gut biome from your mom. The total number of genes present in the microbes of your microbiome is 200 times more than your genome. Nearly 1000 species of bacteria inhabit your gut biome most of which are beneficial for health. Gut-friendly bacteria help in digestion and regulation of immune system and protect us from harmful microbial invasions. It also helps in the synthesis of Vitamin B and K.
Dysfunction of the microbiome is responsible for autoimmune diseases like diabetes, muscular dystrophy, rheumatoid arthritis, multiple sclerosis and fibromyalgia. Since people inherit microbiome, autoimmune diseases might be passed through this route, not by DNA. An unbalanced gut microbiome causes inflammation, the root of all chronic ailments. A healthy gut not only can keep chronic ailments at bay but may also reverse it.
How to let food be thy medicine?
This ancient philosophy propagated by Hippocrates holds to a great extent even today. What you eat affects your gut. Breaking down of food in the gastrointestinal tract creates lots of products that may or may not support gut microbial colonies. Some foods might release toxins and create inflammation in some individuals while with others it may not be the same. It is all about the power of microbial colonies lining the gut, and correct food can strengthen your gut biome.
How gut biome supports your health?
Fighting for your good:
Your gut microbiome is in a constant battle with bad bacteria. They multiply frequently to check the proliferation of the harmful class. A balanced gut microbiome population keeps you healthy. If the balance gets disturbed, you are likely to suffer from:
- Irritable Bowel Syndrome
- Ulcerative Colitis
- Crohn’s disease
Researchers are looking for different treatment approaches by targeting the gut microbiome colonies.
Gut biome may influence your immune response
Recent studies conducted in 206 Covid-19 patients with less severe respiratory symptoms but marked digestive symptoms produced interesting results related with gut biome. Poor gut biome may be responsible for poor immune responses of the gut and also of distant mucosal sites that is lungs.
Gut health and your heart:
Some kind of gut bacteria may have a link with blood cholesterol that can affect your heart health. On taking red meat or eggs, bacteria synthesize a chemical which is converted to TMAO (trimethylamine-oxide) by the liver.
TMAO leads to building of plaque in blood vessels. So if that harmful colony can be eliminated, would you at all need to be scared of consuming eggs and red meat? According to research studies, DMB, a natural substance present in olive and grapeseed oil can restrict TMAO production. The same TMAO can cause chronic kidney disease if people cannot get rid of it.
Gut biome has lots to do with your obesity:
You may need to address your obesity differently. Researchers have found certain amino acids in our blood can be linked to obesity and gut biome composition. Gut biome affects our body metabolism and may contribute to obesity and Type 2 diabetes.
Earlier researches have shown people suffering from these diseases have a varied range of metabolites in the blood. In-depth studies identified 19 different metabolites that can be associated with a person’s BMI. Of them, the glutamate and branched-chain aromatic acids (BCAA) can be highly linked to obesity.
Again, these obesity-inducing metabolites can be linked to four different kinds of gut bacteria. So, if your gut biome has a higher population of these colonies, you are likely to be obese. In future, researchers aim to alter the gut biome composition to reduce the chances of metabolic and cardiovascular disorders.
Control of blood sugar lowering the risk of Diabetes:
A drop in microbial diversity in the gut can increase the risk of diabetes as revealed by some studies. It was found that the levels of unhealthy bacterial communities surged just before the onset of Type 1 diabetes.
The gut-brain connection:
We have felt it but not quite acknowledged it. Though gut and brain are far apart, they are connected 24X7 through a two-way biochemical communication channel. Gut-wrenching experience, butterflies in the stomach and feeling nauseous to certain incidents do provide an explanation of the gut-brain connection.
Special nerve cells and immune pathways form the gut-brain axis, the smart way to communicate. Your gut can produce neuroactive compounds that include 90% of serotonin, a vital neurotransmitter. We all know the role of serotonin in regulating our emotions. Sometimes the gut sends signals to the brain. It is also known as the ‘second brain’ and these two brains do talk to each other.
For decades, researchers thought anxiety and depression contributed to digestive problems but it can be the other way round, intestinal distress can cause anxiety and depression. Researchers are gathering evidence that gastrointestinal irritation may cause mood changes. It sends signals to the Central Nervous System. This might explain why higher than average percentage of patients suffering from IBS and functional bowel problems suffer from anxiety and depression.
These recent findings are providing a newer approach to treating gut ailments, for example, prescribing antidepressants. This is not meant for the brain cells but may also calm the nerve cells lining the gut. Similarly, CBT can be suggested to improve the brain-gut communication.
Unhealthy gut microbiome may contribute to Alzheimer’s and other related conditions leading to dementia. In a sampling study, it was found people with Alzheimer’s have a unique gut biome, which is a less diverse community of microbes than that found in healthy people. The gut microbiome can affect your cognitive function.
Recent research found that the transplantation of microbes from some young animals to old animals led to the rejuvenation of some aspects of immune and brain function. Research published by the group APC as well as some other international groups have detected that gut microbiome plays an important role in the aging process and aging.
Thus, having a good microbiome could potentially lead to reversal of age-related deterioration of the brain. As the studies observed improvement in cognitive function and learning ability, the importance of microbiome or gut health cannot be ignored, though more studies are required for these findings to be true for humans also.
Mother’s microbiome can affect brain development in kids:
A groundbreaking research states, mother’s microbiome is a key contributor to several neurodevelopmental disorders in offspring including autism. Days are not far when a pregnant mother’s microbiome would be analyzed to assess the risk of the autism in the unborn child. According to the CDC, 1 out of every 59 kids in the US is diagnosed with autism. The number is up from 1 in 150 in 2000.
Interestingly, a revolutionary technique called Microbiota Transfer Therapy has shown remarkable improvements in autism treatment. After two years of treatment, a 45% drop in the core ASD (Autism Spectrum Disorder) symptoms regarding language, behavior and social interaction has been observed.
Do you have a healthy gut?
The golden rule, more diverse the gut biome healthier is your gut. It is regarding both the population strength and diversity. Gut health diagnostic testing helps in estimating the diversification of your gut metropolis. Labs with cutting-edge facilities are helping with such tests by providing insights into why IBS, GERD, constipation and other digestive problems are occurring.
Sometimes people with underlying gut problems do not feel any symptoms at all but there may be ripple effects like immune, metabolic, hormonal and brain issues. For example, nearly 22% of people suffering from celiac disease do not suffer from any gastrointestinal problem but there may be significant damage in the small intestines.
Personalized nutrition – the key to a healthy gut:
Taking the right kind of food is the key to maintain your gut health. The one-size-fits-for-all approach does not work. Given the uniqueness of gut biome of every individual, food suitable for your gut biome may not be suitable for your sibling, parent or anybody in the family. Proper analysis of microbial colonies in your gut would help in creating the right diet plan for you.
Gut biome companies are creating personalized nutrition plans based on individual gut biome analysis but it is yet to go mainstream. Research is on to confirm the metabolic activities of different gut microbes towards different types of food.
It is not only the food to be considered. Other factors like environment and lifestyle also need to be assessed in the diet plan. All these have a direct influence on the gut microbe community of an individual.
Take more of Probiotics and prebiotics:
Probiotics present in some food reinforce the microbe community in your gut. All probiotic foods do not work in the same way. Each kind has its way of functioning and the effects are different. They boost immunity and strengthen the gastrointestinal tract especially of those with IBS.
You get them in plenty in live cultures of lactobacilli and bifidobacteria. Yoghurt, kefir and aged cheese are good sources. You can find them in fermented vegetables like kimchi, gherkin, sauerkraut and pickled vegetables.
To improve the mouth microbiome, spinach, celery and beetroot juice have been found to be beneficial. These foods promote the bacteria that is associated with brain function and healthy blood vessels, as they are packed with inorganic nitrate.
Care more for your oral microbiome – Say goodbye to your toothpaste
Some products developed for oral hygiene such as toothpastes and mouthwashes have a heavy concentration of alcohol, or essential oils which are harmful for your mouth microbiome. This destroys the microbiome in the mouth. So check the composition of your toothpaste and change to one which is prebiotic or probiotic, to retain the good bacteria in your mouth.
Lactobacillus has high potential in boosting immune response restoring gut homeostasis
In the current scenario, when the world is struggling for a cure to the deadly pandemic virus, few are paying attention to the potential of Lactobacillus in improving body immunity. Acceptable scientific data with Lactobacillus strains show improvement in respiratory infection treatment outcomes. Studies have also shown that it also helped in reducing respiratory viral infections in the elderly people.
Another study conducted in 742 children showed a reduced risk for nosocomial gastrointestinal and respiratory tract infections in pediatrics. The potential of lactobacillus has also been substantiated in a study among mechanically ventilated patients where use of lactobacillus reduced the incidence of developing ventilator-associated pneumonia among high risk ICU patients. Orally administered probiotic strains can also reduce the severity and incidence of respiratory tract infections.
Prebiotics boosts the function of probiotics. They may help in better calcium absorption as well as improve your gut health. Bananas, onions, almonds, leeks, asparagus, garlic, soybean, artichokes and whole wheat are few of the examples. You can combine prebiotics and probiotics to make it synbiotic like having a banana with yoghurt or stir-frying asparagus with onions.
Physical exercise:
Recent studies have also pointed out that regular physical exercise can bring changes in specific bacteria and its metabolic activities. This is attributed to several physiological functions that occur while exercising, like change in body temperature, enhancement of blood circulation, activity changes in the nervous system and energy output.
All these lead to certain alterations to the intestinal bacteria leading to a reduction in inflammation and oxidative stress. It further benefits the brain and muscle tissues and protects our body from IBS and colon cancer. Exercising has far-reaching effects on gut bacteria more effective than probiotics and supplements.
Depend on antibiotics less:
Trust your inherent healing power. Avoid taking antibiotics for every small ailment. Antibiotics kill gut-friendly microbes along with the infection-causing strains. While on antibiotics, make sure to take lots of probiotics to boost the growth of beneficial microbes in your gut.
Other ways to restore your gut health:
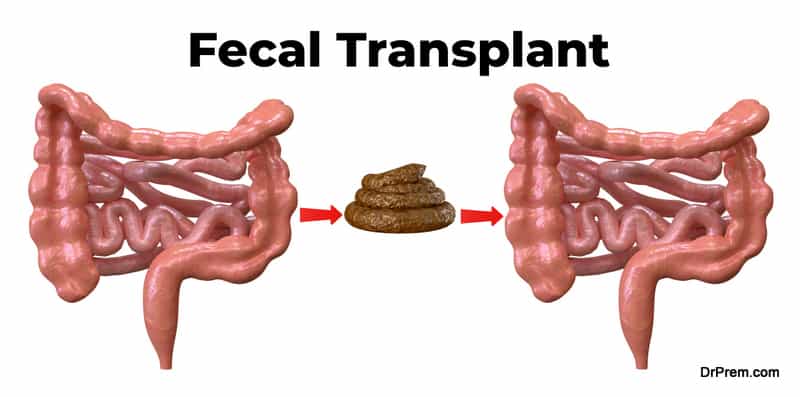
Fecal Transplant:
In this technique, feces from a healthy donor are transplanted into another person to restore the healthy balance of gut microbes. It may also be purposed to introduce colonies of special bacterial strains from the donor’s feces to the recipient lacking those specific strains.
Lack of microbial diversity or absence of specific bacterial strains in the gut can give rise to certain ailments. It is a unique way of facilitating quicker recovery without any expensive or complex medical interventions.
Nearly 20% of people taking antibiotics for treating Clostridium difficile, a common digestive tract infection like diarrhea, are likely to face recurrence. Antibiotics may disrupt the gut microbe balance. In such cases, a fecal transplant can be a good option. Recently, it is being considered to treat autism in kids.
Typically, the donor feces are transplanted to the recipient by colonoscopy. Applying enema can be another way of fecal transplantation. Fecal transplant is an age-old concept rooted in ancient Chinese Medicine. Today, the methods are safe and are supported by evidence-based research.
Deep Transcranial Magnetic Stimulation (dTMS):
The non-invasive dTMS can help in weight loss for obese persons by partially changing the gut bacteria. Impaired gut microbial composition is one of the underlying causes of obesity which can alter the brain’s signals related to food cravings, appetite and satiety.
dTMS is not an invasive procedure. An electromagnetic coil is placed over the scalp which sends magnetic impulses to activate specific centers in the brain. This technique approved by the FDA is currently used to treat depression. Recent findings of applying dTMS on obese participants found, it also improved the composition of intestinal microbes.
Final thoughts:
Interesting findings on gut biome and its correlation with our health and wellness are creating ways for innovative treatment approaches that were never conceived of. Personalized nutrition would be the basic norm of healthcare, not for cure but prevention. Gut biome may be considered an important biomarker in disease prediction and treatment. For a healthy gut, it is always recommended to stick to the basics like having more probiotics and regular exercising. Sickness automatically becomes an option, not a mandated misfortune.