How aware are you about infections in medical tourism that can happen due to many reasons? Whether you are a patient or any medical tourism business, you need to have a good understanding of this and take adequate measures. Infections can be mild or serious, which may again vary from patient to patient. Endemic diseases tolerant to the local population may turn out fatal for foreign patients.
In this guide you will read about:
Guide on How to Take Protection from Infections in Medical tourism: Tips for patients, hospitals and other facilities
-
Common infections in medical tourism
-
How to protect against infections
-
Importance of immunization
-
How to protect yourself from various infections during medical tour
-
Why Medical tourism hospitals should go for AMR checkups?
-
How does AMR spread?
-
AMR infections: How threatening it is for medical tourism?
-
Misuse of antibiotics
-
Few new antibiotics are in the development process
-
How medical tourism is facilitating the spread of AMR infection?
-
Healthcare strategies to combat AMR in Medical Tourism
-
Steps medical tourism hospitals should take to prevent AMR
-
Maintaining health-hygiene and other preventive methods
-
Have a well-framed antibiotic policy
-
Identifying patients who are at high risk of infection
-
Utilize the hospital’s antibiograms
in Medical Tourism
-
Use microbiology tests to check AMR infection
-
Surveillance of antimicrobial resistance in Medical Tourism
-
Development of Standard Treatment Guidelines (STG)
Common infections in medical tourism
One of the most common illnesses medical travelers face is the traveler’s diarrhea and the major reasons for this ailment is the ingestion of certain organisms found in contaminated food or water. Anxiety, allergies and dietary changes could also be the reason for traveler’s diarrhea. Other travel-related health issues include malaria, dengue, yellow fever, hepatitis A, hepatitis B, typhoid fever, and cholera.
In a foreign land, the infections can occur due to many reasons. Even a small allergy, if left ignored, could potentially trigger serious infections. The most common vector-borne diseases are the yellow fever and malaria. It is important to note that if you do not receive the right treatment for such diseases, they can turn fatal. If proper medication is on hand, you could avoid any further damage to the body.
In case of certain infections, the old adage “prevention is better than the cure” holds true. Prevention from infections is not easy. It is even more difficult for people who are already suffering from diseases. It is particularly important for patients who intend to undergo surgery in a foreign land to follow strict guidelines, as they are at an increased risk.
Medical tourists should have the necessary information on how to stay healthy and how to self-medicate or seek medical help in case they contract any disease in the foreign country. Medical preparation is even more important if you are traveling to a country where vector-borne diseases are widespread. When it comes to prioritizing travel-related health recommendations, a medical tourist should always keep in mind the risks of travel-related illness and the importance of vaccination and medicine.
How to protect against infections
The first step towards protection against infections is maintaining hygiene.Medical tourists, as they are mostly unfamiliar with the climatic conditions and the region-specific ailments in a particular destination, are always at a greater risk of falling sick when compared with the natives of that particular country.
Usually, the locally or internationally accredited medical facilities tend to follow strict hygiene and sanitary requirements. It is useful to determine whether the hospital or clinic where you are seeking care has received proper accreditation. Checking for the hospital’s accreditation is an important step in determining the standards of hygiene and the healthcare services provided by the facility.
Importance of immunization
Before you embark on your medical trip, it is important to discuss your travel plans in detail with your local or treating doctor, as well as the medical tourism facilitator company, who can also guide you.The concerned doctor can then make recommendations, considering the patient’s age, medical history, vaccine history, destination and the length of the trip. When it comes to medical tourism, proper vaccination plays an important role in protection against a number of infections in a foreign country. In some cases, your local physician might refer you to a travel medicine specialist for detailed information on travel medicine.
The process of vaccination usually consists of a few steps. Medical tourists should always undertake the entire immunization process prior to traveling, as it is important to ensure that the vaccine will work as desired. You must ask your travel medicine physician about the vaccination you will need for protection against food- and water-borne illnesses, and other travel-related illnesses.
Although it is important for all medical tourists to consider the significance of vaccinations and medications, you should always rely on safe health practices, such as eating health food and drinking pure water, in order to prevent yourself from various infections. Also ask your medical tourism consultant who can guide you to hygienic restaurants and health facilities.
Many of the diseases are water- and food-borne. Therefore, consciousness about the consumption of street food or tap water is very important in preventing certain diseases.
Some countries might ask for the proof of vaccination required to enter the country. For example, if you are traveling to sub-Saharan Africa or other yellow fever areas, you might need the proof of vaccination against yellow fever. Your medical tourism facilitator company can provide you with the details of the vaccinations you need.
While contaminated water and food are the major sources of diseases overseas, a medical tourist should consider many other things for successful prevention of infectious diseases. Apart from food and water, you must also be cautious against insect bites. Mosquitoes can cause a number of life-threatening diseases. You should always carry mosquito repellent as a preventive step against mosquito bites.
Most internationally traveling patients visiting tropical countries are concerned about the possibility of contracting malaria. Tropical countries have a relatively higher risk of mosquito borne illnesses. You can easily find various ointments, creams and pills that could protect you from the danger.
Certification and documents form a very important part of the medical endeavor. When going to a foreign country, carry all the records that certify the immunizations you have received in the past. This will enable the doctors at the medical tourism destination to have a proper knowledge about the kind of drugs and further treatment, so that they can attend to your case appropriately. If the documents are in a language that is not internationally recognized, then it is wise to translate this into a language that is acceptable at the destination.
The common vaccines you may need when going overseas include hepatitis A, hepatitis B, influenza, pneumococcal, polio, rabies, typhoid fever, yellow fever, tetanus and Japanese encephalitis.
Irrespective of the country you are visiting for your medical treatment, you should be up to date on all the routine immunizations you will require for effective prevention against infectious diseases in unfamiliar environments. Even if you have to embark on a medical journey in less than three to four weeks, you should consult with your local doctor to check if you need any vaccines or medicines. In nutshell, the recommendation of the right vaccinations is one of the major components of a pre-travel medical consultation.
How to protect yourself from various infections during medical tour
More than 800 million people travel abroad for different kinds of medical treatment, every year. Medical tourism involves patients crossing international borders more often; it has become essential for potential medical tourists to seek pre-travel suggestion in order to avoid unpleasant situations and stay healthy during the journey.
Every country has different standards of healthcare. It is very important for the patient to adhere to the guidelines set by experts in a medical tourism destination in order to stay fit and healthy during the trip.
Preparations
As a medical tourist, you should get familiar beforehand with the different conditions at a particular destination that could have bad effects on your health. You should take care of all these things, such as pollution levels, standards of healthcare services, necessary immunizations or vaccination and the availability of medical supplies. You should prepare a complete travel medicinal kit along with the other essential travel- related things you plan to carry to the foreign destination.
Protection
There are many medical tourism locations where the chances of contracting infectious diseases are considerably high. One of the most common illness medical traveler faces is diarrhea. The major reason for this ailment is the ingestion of certain organisms found in contaminated food and water.
Even though protection from infections is not easy, still you can protect yourself from these infections with little care and attention. One of the main reasons for large number of infections is the lack of hygiene, so it is important to maintain hygiene.
Immunization
It is important to discuss your travel plans in detail with your local physician. Immunization is process by which the immune system of an individual becomes prepared against the potential disease. Medical tourists should always undertake the entire immunization process prior to traveling. It is important to ensure that the vaccine will work properly as a defense against the potential disease in a particular destination. A Medical tourism consultant can advise you about the prevalent diseases that you need to protect yourself from.
Travel medicine kit
It is important to prepare a travel medicine kit. You must sure that the kit has enough medicinal supplies to prevent common infectious, such as illness and minor injuries.
Why Medical tourism hospitals should go for AMR checkups?
The rising incidence of travelers carrying Antimicrobial Resistance (AMR) infections during repatriation may cast a shadow on medical tourism. Medical tourism hospitals need to arrange AMR checkups for better patient outcomes. Incidences of AMR infections and associated complications are creating fresh doubts in medical travelers.
- Are we safe from drug-resistant infections in foreign healthcare settings?
- Do hospitals have the required infrastructure and follow recommended practices in AMR prevention and treatment?
Antibiotics are life-saving but its misuse can be killing. An estimated 700,000 people worldwide die from it every year and failure to curb it would result in 10 million deaths by 2050 surpassing the global cancer death number of 8.2 million.
When drug-resistant microbial infections fail to respond to treatments, it prolongs illness, increases treatment cost and heightens the risk of death. Failure to treatments also results in extended periods of infections raising the chances of spreading the same in the community.
How does AMR spread?
- Individuals taking prescribed antibiotics may develop AMR as a natural adaptive reaction and may spread it to other persons.
- Antibiotics prescribed during the hospital stay can also cause AMR and spread to other patients via contaminated objects and unclean hand touch.
- Patients carrying resistant bacteria after getting released from the hospital can spread to other persons in the community.
- Traveling to a country with a high prevalence of AMR increases the risk of AMR contamination.
First-line antibiotics previously effective in such patients cease to be effective in patients with AMR calling for second-line antibiotics. It cannot be ensured that the last line antibiotics can provide the necessary cure in saving the patient’s life.
AMR infections: How threatening it is for medical tourism?
Misuse of antibiotics
Hardly there exists any treatment that does not require antibiotics. Consider the large fraction of medical tourists traveling to other countries seeking a range of affordable surgical treatments in foreign countries. Doesn’t it expose them to antimicrobials and associated AMR infections?
Growing evidence collection suggests widespread overuse of antibiotics in most healthcare settings is responsible for AMR. Medical tourism has the potential to spread it more in case of inadequate AMR prevention strategies in hospitals/clinics.
Limited regulation in antibiotic usage, the ready availability of over-the-counter antibiotics, poor sanitation and overcrowding are common in some developing nations also popular for medical tourism.
Few new antibiotics are in the development process
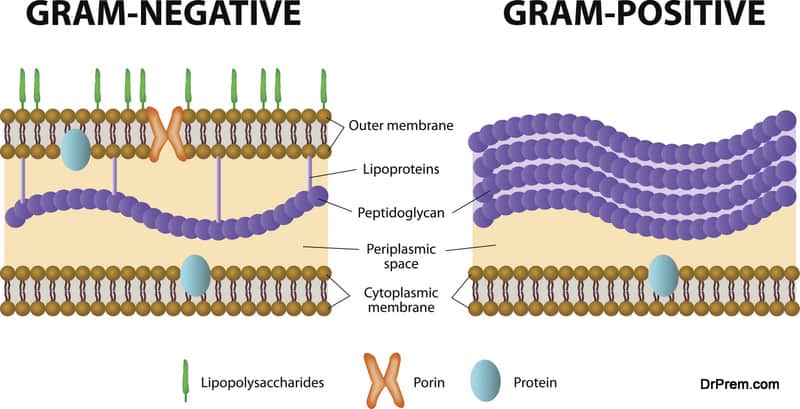
New antibiotic development has dropped sharply since last two decades. No new classes of antibiotics to treat gram negative bacilli are available for the last 40 years. Physicians have limited arms in their arsenal.
If optimal antibiotic usage is not practiced, medical tourists would be at a higher risk of contacting AMR infections. Medical tourism hospitals/destinations need to realize this soon else it may jeopardize the growth in this sector.
How medical tourism is facilitating the spread of AMR infection?
A considerable number of patients carrying drug-resistant infections had a previous history of traveling abroad. They may be either medical travelers or vacationers forced to medical treatments in the foreign country owing to an accident or sudden illness.
Although data shows that the number of intended medical travelers infected with AMR is very low but this cannot be considered as a relief factor. Indeed, medical tourists are more aware of risk factors. They do more research and gather authentic information from reliable sources before deciding on the destination or facilities.
But is that enough? Healthcare facilities also need to provide thorough information of their AMR prevention strategies to win trust and confidence of foreigners.
Healthcare strategies to combat AMR in Medical Tourism
Global healthcare is still grappling to prevent the spread of multidrug-resistant Gram-negative bacteria. Although countries have stepped up efforts serious gaps remain. Some European nations have been working on this for over four decades while others have recently launched their action plans to control the growing threat.
High-income countries are much ahead in the progress and implementation of AMR policies than the low-income countries. But a majority of medical tourism business activities are happening in developing nations. This poses a greater threat of AMR infection.
Healthcare facilities need to formulate a strategy which would include:
- Educating patients and physicians about proper the proper drug, its dose and duration.
- Promoting judicious use of antimicrobials in healthcare settings.
- Monitoring drug intake adherence.
- Implementing effective infection-control practices to prevent the spread of AMR infection from the infected patient to non-infected ones.
- Establishing foolproof antimicrobial surveillance
- Enhanced use of immunization
- Developing and implementing an Antibiotic Policy and Standard Treatment Guidelines
- Adequate planning for identifying, transferring, treating, discharging and readmitting patients with colonized AMR infections.
- Monitoring AMR and providing feedback about it.
- Campaigns to create public awareness about the dangers of AMR and what could be done to tackle it.
Steps medical tourism hospitals should take to prevent AMR:
AMR is likely to be a community-driven problem where a significant population may be carrying antimicrobial-resistant germs. Similarly, medical travelers coming from different countries can also be the carriers. Hospitals attending international travelers can take several steps to prevent antimicrobial resistance:
1. Maintaining health-hygiene and other preventive methods
A considerable number of physicians in a survey feel poor hand hygiene as one of the leading causes of anti-microbial infections. Most surveys of hand-washing in various patient-care settings reveal appropriate hand washing practices exist in only 25%-50% opportunities. Hospitals should improve hand washing practices by enforcing the use of alcohol-based hand-rub and disposable examination gloves with regular surveillance in operation.
Other methods include isolating the infected patients and proper cleaning and disinfection of the environment and equipment.
2. Have a well-framed antibiotic policy
Does the patient require antibiotics at all? This is the first and foremost issue to be addressed in all cases be it domestic or international travelers. Such an approach sets a culture for optimal antimicrobial use. This should be applied at the prophylactic phase as well. The hospital antibiotic policy should be evidence-based and align with the national antibiotic policy barring a few changes as warranted by the local antibiotic resistance profile.
The policy should include:
- The range of antibiotic activity
- Pharmacodynamics of the drugs and its adverse effects
- Potential to selective resistance
- Cost
- Special requirements of individual patients/groups
- Set the level of antibiotic prescription. First-line drugs can be prescribed by all physicians while specific ones can be prescribed only after due consultation with the antimicrobial team head.
The team formulating antibiotic policy must be from multiple disciplines and perform important functions including scheduling antimicrobial regimen, monitoring drug therapy, discontinuation of prophylaxis antimicrobials, approving restricted antimicrobials, suggesting additional laboratory testing and others. The policy should be reviewed periodically incorporating updated medical knowledge, clinical practices and local situations. This practice would boost medical tourism business and lead to economic benefits.
3. Identifying patients who are at high risk of infection
Screening of patients is a useful way to identify patients carrying AMR infection. They can be segregated and treated in isolation. Before putting them on antimicrobials, hospitals should go for cultures and target empiric therapy based on the progress of the disease.
4. Utilize the hospital’s antibiograms in Medical Tourism
Antibiograms constitute a periodic summary of antibiotic susceptibilities to locally isolated bacteria in the hospital’s repository of clinical microbiological reports. Clinicians often refer these reports to assess the susceptibility rates. This helps in selecting empiric antimicrobial therapy and monitoring resistance trends developing over time within the particular healthcare setting.
5. Use microbiology tests to check AMR infection
A multicenter cohort study conducted in hospitals of West Norway concluded microbiology tests can have a positive influence on patient outcomes and limit the use of broad-spectrum antibiotics.
Unfortunately, the potential of these tests is yet to be fully utilized in healthcare settings. Hospitals can review the existing pattern of ordering microbiology tests and utilize the test reports in a more targeted and overarching approach.
6. Surveillance of antimicrobial resistance in Medical Tourism
Mandatory inclusion of antimicrobial stewardship program to monitor antimicrobial usage, improve patient outcomes, reduce incidences of AMR infection and prevention of its spread. It should:
- Be able to predict the evolution of antimicrobial resistance
- Monitor antimicrobial consumption
- Measure of antimicrobial consumption in accordance with the daily defined dose (DDD) of the Anatomic Therapeutic Chemical (ATC) classification system.
The program is an ongoing process of systematic data collection followed by analysis and interpretation for successful implementation and evaluation of clinical practice.
Therefore, a standard surveillance system should have the following features:
- Laboratories should maintain a definite standard in reporting quantitative AMR data.
- They should generate a reliable numerator discarding duplication of data.
- Participate in routine quality assessment programs for proficiency testing.
- Employing well-trained microbiologists
- The selection of microbes and antimicrobials should be based on its implication on public health.
- Apart from laboratory data, inclusion of clinical data.
- Flexibility to accommodate changing information and inclusion of new data related to new AMRs and health conditions.
- Use of the open-source software with the WHO, WHONET for seamless data entry and analysis.
Development of Standard Treatment Guidelines (STG)
STG helps in bringing a change in treatment approach and clinical behavior impacting more positive outcomes. Physicians should be involved in the ownership of guidelines.
The guidelines should be based on:
- Local antibiograms
- Syndromes and symptoms
- Clinical settings – outpatient, in-hospital or ICU
- Strong rationale
- Evidence-based recommendations
Medical tourism growth has picked up. Apart from offering affordability, quality and comfort in services, destinations should emphasize on AMR checkup facilities and infection prevention. They should ensure safe homecoming of patients free from any bug.