You are sick. You visit a doctor and request a course of antibiotics for a quick cure. If the doctor is unwilling, you go to a pharmacy and take antibiotics according to their suggestion. Not only this, when you feel cured after taking a few doses, you stop taking the full course. This is a dangerous practice. Hardly, you know that misuse or overuse of antibiotics can be killing.
Antibiotics have played a great role in treating varied microbial infections, but you also need to know when they are useful and when they can be dangerous. Some studies project that by 2050 antibiotics overuse can be responsible for 10 million deaths every year worldwide surpassing cancer.
Antibiotics are meant to kill bacteria not virus:

We fall sick primarily due to two microbes, bacteria and virus. Common infections like flu, cold, bronchitis, sinus and ear infections are caused by the virus. Antibiotics not required treating viral infections; symptom relief measures are enough to treat these infections. We are not even aware of our immune power where antibiotics have nothing to do.
Certain viral and bacterial infections have similar symptoms but the way they spread is different. Our body is a host of numerous bacterial colonies that are mostly beneficial. Some harmful colonies may start multiplying causing serious infections. The virus does not exist in our body but invades through external agents. Our body immunity can ward off many such infections.
Why should we be concerned with antibiotic overuse?
The following reasons should make doctors and patients think twice before reaching out to antibiotics:
-
Increased incidences of fatal diarrhea in children:

Antibiotic-resistant bacterial strains C.diff is responsible for 250,000 hospitalized infections causing 14000 deaths of children and adults annually. A study found, 71% of children affected with C.diff were previously treated with antibiotics for ear, nose and respiratory ailments which were not required.
-
It can upset the healthy gut microbial balance by killing good bacteria
Antibiotics not only kill harmful bacteria but also the friendly bacteria in your gut and disrupt the healthy gut bacteria balance. A healthy balance of gut bacteria is essential to maintain our normal body functions.
-
Beneficial bacteria can turn bad.

Your good bacteria in the gut can turn bad by cohabiting with the bad bacteria. Bacteria do not always pass their genetic traits through bacterial reproduction. They can just pass it to their fellow colonies just like students pass class notes to their classmates in the classroom.
-
It can lead to antibiotic resistance, a growing health menace across the globe.
The overuse of antibiotics is reflected in the growing number of antibiotic-resistant infections from 2002-2014. Many of these are untreatable.
-
Increased cases of antibiotic resistance mean higher treatment and hospitalization costs.

Since 2002, healthcare costs in the US have shot up by $1383 per case of infection costing $2 billion annually. This is because the infections become complicated and demand intensive drugs and longer hospitalization period.
Antibiotic overuse is killing us:
 Antibiotics have been saving millions of lives since its discovery. In the course of time, its overuse has created drug-resistant bacteria. This implies that common antibiotics will no longer be effective in curing the same disease. A patient suffering from a specific bacterial infection will not respond to the first line of antibiotics.
Antibiotics have been saving millions of lives since its discovery. In the course of time, its overuse has created drug-resistant bacteria. This implies that common antibiotics will no longer be effective in curing the same disease. A patient suffering from a specific bacterial infection will not respond to the first line of antibiotics.
It will need stronger antibiotics, which means higher cost and prolonged treatment period. Even the second line of antibiotics may not be effective and the infection can be fatal in the end.
Over prescription and unregulated use of antibiotics:
At the initial stage of discovery, antibiotics were prescribed when nothing worked. It used to be the last resort. Surprisingly, this approach has changed. Pharmaceutical companies are manufacturing antibiotics in huge volumes. It has become easily accessible to many. Therefore, we are free to take antibiotics for simple maladies. Between 2000 and 2015, the use of antibiotics has doubled globally as reported by the study from the Center for Disease Dynamics.
We have developed too much dependence on antibiotics. Over prescription is another big reason. The Centers for Disease Control and Prevention found at least 30% of antibiotics prescribed were not necessary. In many low and middle-income countries, the use of antibiotics is not regulated. It can be purchased without any prescription.
5 deadly antibiotic-resistant bacteria creating global health havoc:
The more we take antibiotics the more it gets normalized in our system and faster the emergence of its resistance. The bacteria residing in our body get acclimatized to it. The deadly consequences that we are facing are as follows:
-
Salmonella typhi:
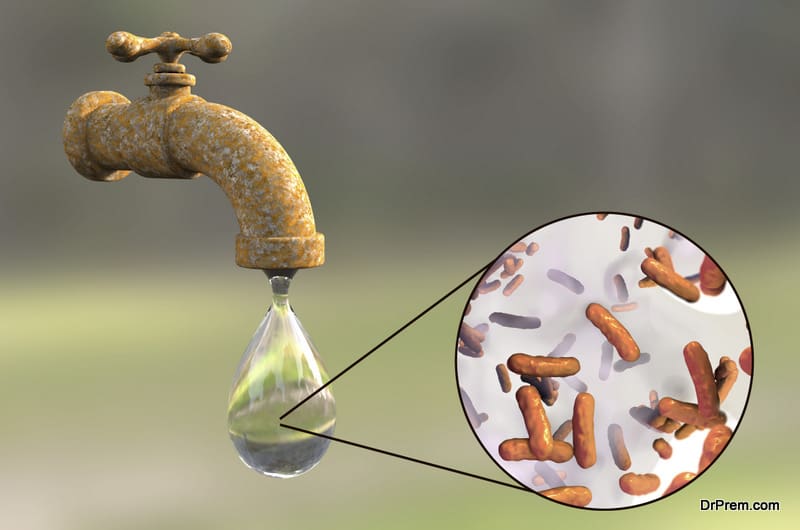
This highly contagious typhoid-causing bacterium affects around 21 million of the global population annually killing nearly 1% of the affected. A drug-resistant strain of Salmonella typhi has evolved. It is resistant to minimum three classes of antibiotics and can be treated only by azithromycin. It is just one step away to be rendered untreatable by all kinds of antibiotics available.
-
Mycobacterium tuberculosis:

The reason tuberculosis has become a global healthcare burden is primarily due to its drug-resistant nature. Mycobacterium tuberculosis kills 1 million people every year. Mycobacterium can easily hide in the cells making it difficult for the antibiotic to work effectively. An estimated 13% of new TB cases are multi-drug resistant which means prolonged treatment schedule, and more unwanted side effects.
The success rate of treating extensively drug-resistant TB is only 30%. The rate at which this form of TB has spread to more than 123 countries is highly concerning. Failing to adhere to a medication schedule is one of the reasons for TB becoming drug-resistant causing further spread.
-
Pandrug resistant Klebsiella pneumoniae:
This type of bacterium is present in the skin and intestine and can cause deadly infections in people with compromised body immunity. It is one of the prime hospital-acquired infections and a critical drug-resistant public health threat.
In 2013, this multi-drug resistant bacterium was responsible for 8000 deaths in the US alone contributing to 50% of death rates in people carrying this infection. Another strain was identified in 2016 which is resistant to all commonly available antibiotics and is almost untreatable.
-
Pandrug resistant Pseudomonas aeruginosa:
This is another type of bacteria with the potential to cause deadly infections in people with poor body immunity and is also one of hospital-acquired infections. Around 51,000 infections are reported in the US every year causing nearly 400 deaths.
Hospitals in England have also reported about 29 cases of Pandrug resistant Pseudomonas aeruginosa for last five years. It is also responsible for deaths from cystic fibrosis. Over 42% of patients suffering from cystic fibrosis could be treated with colistin in 2013. This is the last line antibiotic since it has become resistant to other antibiotics available.
-
Neisseria gonorrhoeae:

Nearly 78 million cases of gonorrhea, a sexually transmitted disease affecting males and females caused by Neisseria gonorrhoeae are reported worldwide. This is usually not serious but if left untreated can cause permanent damage.
But about one-third of these infections have become resistant to at least one antibiotic. What is more worrying is that a new strain, an extensively drug-resistant one has been identified which can spread fast in a population where people have sex with multiple partners.
We should worry about antibiotic resistance:
If antibiotics lose their effectiveness, this means have lesser arms in our arsenal. Bacteria are adapting themselves in unique ways to survive the antibiotic assault. They are developing different types of resistance mechanisms that can be shared with different bacterial strains resulting in its spreading.
The result, global population is facing a frightening situation where about 1 million people die every year from bacterial infections not treatable with commonly available antibiotics.
So what lies ahead if things are not checked right now?
-
We will run out of antibiotics:

We might have to go back to the early healthcare system where simple cuts wounds that we consider so simple can turn fatal. Pneumonia, a common illness will become untreatable. Imagine the time when people used to die in numbers owing to lack of suitable antibiotics.
-
Future outbreaks can be dangerous:
Drug-resistant bacteria can pass their genes to other strains making them drug-resistant as well. It can affect community health leading to dangerous outcomes.
-
No new antibiotics are coming up:

New classes of antibiotics are not coming up in the market for quite some time. So we need to ensure to create situations so that the existing ones remain effective. Even if new antibiotics are discovered, there is no guarantee that these will not become ineffective to bacterial adaptation mechanisms.
-
Antibiotic resistance is not a future concern:
It has started showing its effects. It is not only about the frightening future, but the current situation is alarming enough. An estimated 25,000 people die in Europe every year from antibiotic resistance. In the US, it is 23,000 every year. If not tackled, the number will shoot up exponentially.
-
Surgical procedures will carry more risk:

Complex surgical procedures always carry the risk of infection. Cardiac bypass surgery or orthopedic operations need antibiotics to deal with infections. If we do not have enough effective antibiotics, many surgical infections may end in fatality.
-
Advanced medical procedures may get stalled:
Take the case of organ transplantation where the patient’s immune system is suppressed to reduce the rejection chances of the transplanted organ. Therefore, a patient might develop bacterial infections for which antibiotics are needed. If our antibiotics do not work properly, the patient’s life is at risk and the procedures may be stalled forever.
-
You can have it in your gut:

You take too much antibiotics even when you do not need them. You run the risk of developing antibiotic-resistant bacteria in your gut. If these bacteria get a chance to create an infection, those antibiotics will not work for you.
Global Anti-microbial surveillance system:

The WHO in 2015 launched the Global Anti-microbial surveillance system creating a standardized guideline for sharing anti-microbial resistant data globally. This is still at the initial stage of implementation. The guideline is a comprehensive set of antibiotic-resistant infection management strategies to be implemented in clinics, hospitals and even at the community level.
It is good that most of the countries have agreed on data sharing but there are chances of discrepancies as well. All countries do not follow the same standards of antimicrobial resistance monitoring and might fail to identify the right pockets of emerging antibiotic infections. Before all these systems come to an acceptable standard, it is wise to tackle the situation at the root. Awareness is a big factor that can create a long term impact.
Appropriate use of antibiotics is the key solution:

Antibiotics affect your immune system. So it is better to avoid them as much as possible. In case of mild illness, allow your body immunity to fight it off. Let your doctor decide whether you need these drugs or not. Your doctor is not supposed to prescribe any antibiotics for common symptoms of cold and flu which can go away by taking analgesics.
Safe practices to avoid antibiotic resistance:

These are applicable to you and your kids too.
- Get a proper diagnosis of symptoms whether it is mild or severe.
- Take antibiotics as prescribed. Do not stop midway.
- Never save antibiotics for future use.
- Never use antibiotics from previous prescriptions
- Do not take antibiotics from other’s prescription
- Practice washing your hands as required and encourage your kids to do so. This will avoid the spread of infections.
Alternative treatments:

If you are diagnosed with viral infections, you have safer alternatives to ease out the symptoms.
- Take over-the-counter medicines prescribed
- Take more fluids
- Take sufficient rest
- To treat nasal congestion, use humidifier, vaporizer or other decongestant nasal sprays
- Gargle with lukewarm saline water several times a day if you have a sore throat.
- Take lozenges, throat drops or even crushed ice to soothe your scratchy throat. Do not give lozenges to your toddler.
- To relieve cough, take honey 2-3 times a day. Kids below 1 year of age should not take honey.
- Treat flu with prescription medicines unless there is any secondary infection.
What lies in the future?

It is scary to imagine a post-antibiotic scenario. Will there be enough antibiotics to fight the resistant strains? The WHO has also set a 2019 deadline to come up with a new class of drugs to fight the superbugs. Researchers are chasing these goals. A new treatment has emerged where synthetic retinoid can be used to treat antibiotic-resistant Staphylococcus aureus instead of antibiotics. But this is still in the research phase.
Till we have a foolproof solution, it is better to be proactive and change our approach to antibiotic use. The responsibility is on everybody – patients, physicians and the government. Next time, you suffer from cold and sore throat, trust your immunity and practice healthy habits instead of trusting antibiotics. It is the pharmaceutical companies that are gaining, not you.



