A recent study conducted by the Vanderbilt University Medical Center in Nashville, TN reveals deep brain stimulation can slow Parkinson’s symptoms. Another research conducted on mice published in Nature Communications a couple of months back states that brain stimulation or activating pleasure centers of the brain causes a rise of “feel good” chemicals. This can positively impact the body immunity system and slow down the growth of tumors.
The finding regarding controlling the Parkinsons’ progression is really exceptional as there is no cure for this disease yet. An estimated 500,000 people in the US are affected by this neurodegenerative disease where elderly citizens constitute a majority of patients, reports Medicalnewstoday. According to the neurosurgery Chief Dr. Ron Alterman, at Beth Israel Deaconess Medical Center, deep brain stimulation in true sense has revolutionized Parkinson’s treatment.
Deep Brain Stimulation (DBS) – a long-term and effective treatment for Parkinson’s:
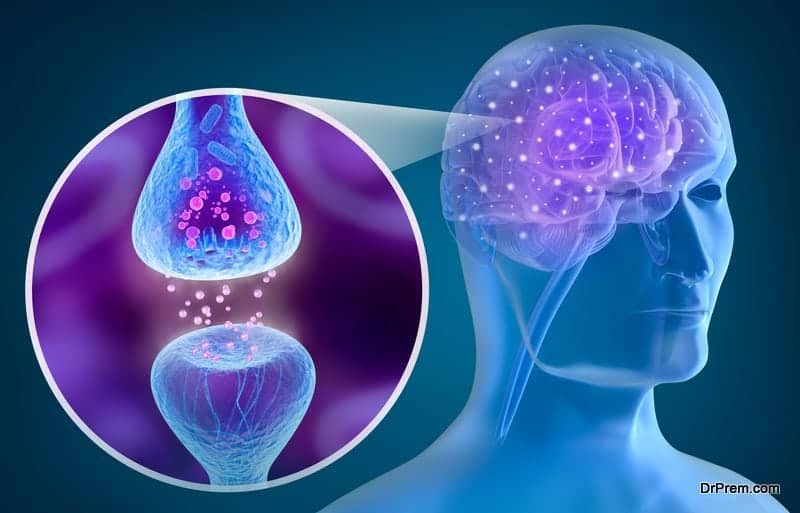
A variety of drugs are administered to alleviate the symptoms of Parkinson’s like tremor, sluggish movement and stiffness but this does not replace the dopamine loss in the brain, the prime cause of the disease. Over time, medications become ineffective.
DBS procedure originated in France in the later part of 1980s as an alternative to brain ablation in which specific tissues of the brain, which were considered responsible for abnormal movements, were destroyed. This is a high-risk procedure with a likelihood of brain damage and paralysis.
The procedure has been carried out since 1997 by Dr. Ron Alterman, Chief of Neurosurgery at Beth Israel Deaconess Medical Center, which is the first hospital in New England to conduct this treatment. Till date, Dr. Alterman has implanted more than 1000 DBS devices. He claims this process keeps patients more functional extending the efficacy of medications.
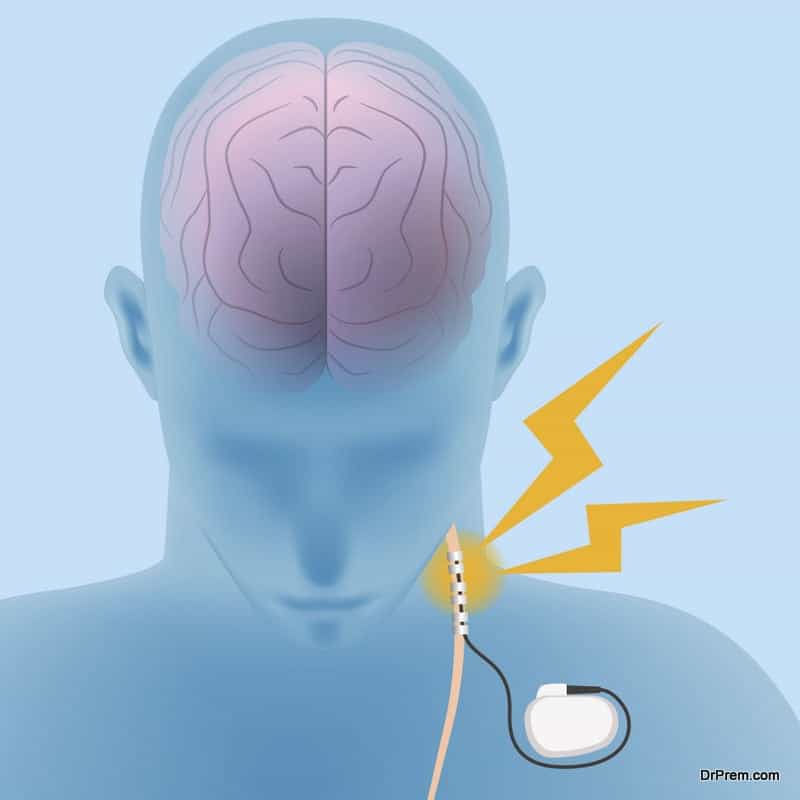
The device and the mechanism:
A pacemaker-like device is implanted under the chest wall to which the electrodes remain connected. The electrodes deliver high-frequency stimulation to the brain, which helps in reducing the tremor. The devices are kept on round the clock and can be shut off in case any difficulty arises. These need to be replaced after every 3-5 years.
Can DBS affect cognitive functions while improving motor functions?

They found that improvements in motor function that slows Parkinson’s symptoms are caused by different neural pathways than those causing unwanted cognitive decline. A better understanding of the treatment mechanism is required to make DBS a more effective treatment by lessening its side-effects.
DBS more effective for early-stage Parkinson’s disease:
Vanderbilt study trial that started in 2006 invited huge controversy as it included participants with early-stage Parkinson’s since DBS was approved only in cases of advanced stage patients when medications fail to control the symptoms. The patients in this study were randomized for a combined drug and DBS therapy and only drug therapy.
The post-clinical trial analysis showed that 86% patients receiving drug therapy alone developed rest tremor in the limbs previously unaffected within the 2-year period while only 46% patients of the combined drug therapy and DBS group developed this symptom. 4 from the DBS and drug therapy group showed improvement in rest tremor while it disappeared completely from all limbs of one patient from the same group.
To test the further effectiveness of DBS and ensure complete safety to the patients, Vanderbilt received FDA nod for a large-scale Phase III clinical trial with 280 people showing early symptoms of Parkinson’s disease. Apart from this, 17 US clinical centers have joined the DBS trial to study its effects on early-stage Parkinson’s.
Chief advantages of DBS:

- The treatment involves minimally invasive procedure.
- The patient’s motor functions improve significantly as revealed after a follow-up period of 7 years.
- Extends the efficacy of medications.
- Requires lesser dosages of medication.
DBS is neither a cure nor it works for everyone but many patients have reported significant improvement with this treatment. The procedure should not be considered as a replacement for medications, it just enhances its effectiveness. Patients showing early signs of dementia due to Parkinson should stay away from this procedure.
Tapping the therapeutic potential of the brain’s reward center in cancer treatment:
Erica Sloan, a biologist at Monash University in Melbourne finds the shift in response to our body immunity to positive influences of the brain’s reward center quite exciting. The communication between the brain and immune system is well established. The biologist, Asya Rolls of Technion-Israel Institute of Technology emphasizes that positive thoughts and emotions can alter the brain’s neural activity.
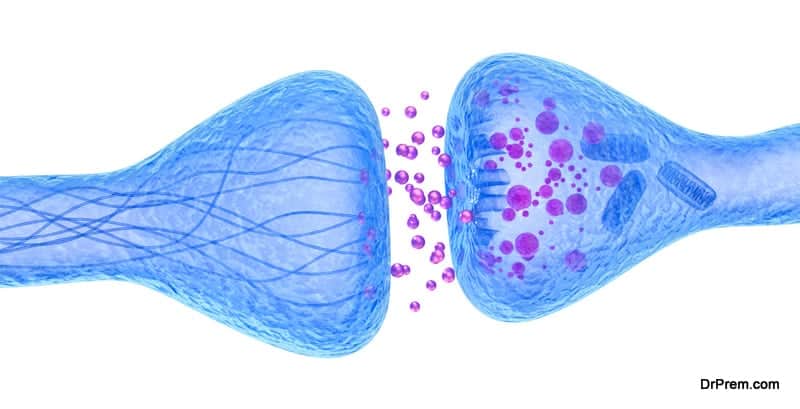
In an earlier study conducted on lab mice, activation of their brain’s reward system resulted in the rise in monocyte count, the group of blood cells responsible for killing pathogens. It is worth noting that monocytes of the brain-activated mice killed pathogens more effectively than those of untreated mice.
The idea of cancer treatment using brain-activation came from a study published in 2014 by a senior co-author. It showed fragmented sleep helped animal tumors grow faster. If disturbed brain (resulting in fragmented sleep) can trigger tumor-promoting activity, it would be reasonable to consider that activation of reward pathway can do the reverse.
This idea was confirmed in a study with mice having implanted cancer cells where a 14-day schedule of daily activation of reward pathway resulted in 40-50% smaller size tumors than those who didn’t receive the stimulation. It can be considered almost equivalent to immunotherapy in cancer treatment. Obviously, the findings come with a warning that cancer patients should not quit medication and only rely on positive emotions.
The above findings clearly indicate the potential for deep brain stimulation in treating untreatable diseases when gene therapy and stem cell treatments are still a long way to come up with effective solutions.